Home
Thanks for stopping by. Pull up a seat and make yourself comfortable…
If you don’t know me already, I’m a speculative fiction writer of mostly flash fiction and short stories, with the occasional novella thrown in. On my publications page, you’ll find the books I’ve been published in, plus a list of other places my work has appeared — either online or elsewhere.
For more information about me as a human being, see ‘about me‘, or for more about me as an author, visit my ‘author press kit‘.
Telling the Bees
A near-future science-fiction novella, published by Newcon Press, 18th July 2023
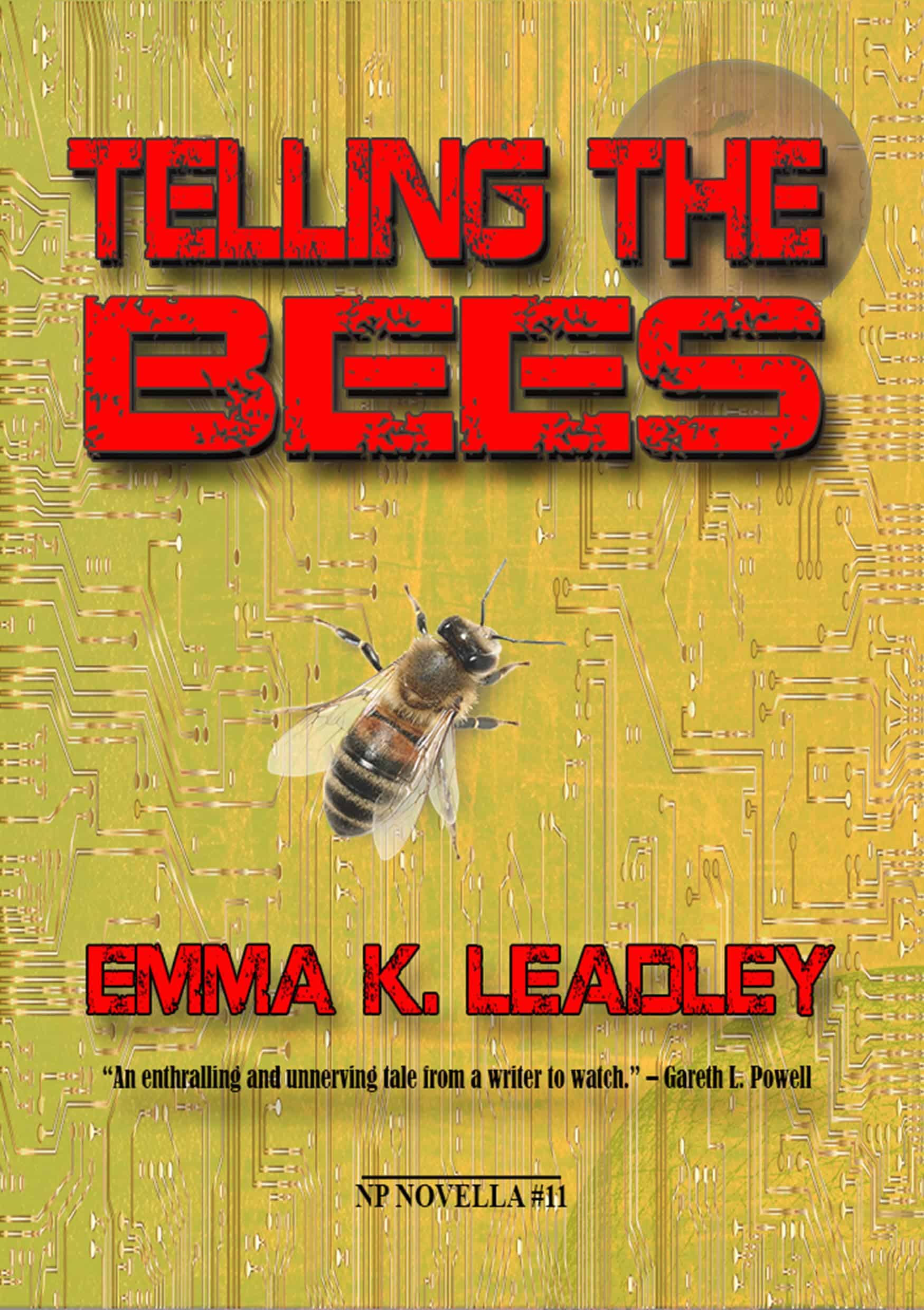
“A smart and fast-paced near future thriller, imbued with reflections on corporate power, emotional bonding and the philosophy of mind… Telling the Bees is cracking entertainment too… The book is a masterclass in concentrated storytelling.” – ParSec Magazine
“An enthralling and unnerving tale from a writer to watch.” – Gareth L. Powell
“A pacy and exciting tale of memory, love and what you’d do to protect what it means to be human. Recommended.” – Stewart Hotston
About Me
Emma K. Leadley
@autoerraticism
Speculative fiction writer, word herder, voracious reader and creative geek. Loves a good pun. They/she.
Subscribe to my newsletter
Telling the Bees
“An enthralling and unnerving tale from a writer to watch.” – Gareth L. Powell
“A pacy and exciting tale of memory, love and what you’d do to protect what it means to be human. Recommended.” – Stewart Hotston